Thyroid Eye Disease
OPENING SUMMARY
- Thyroid Eye Disease (TED) is linked with autoimmune disorder of the thyroid and can present with serious symptoms that can eventually lead to loss of vision.
- At the onset, the active disease phase is characterized by recurrent inflammation reactions that can last for a few months or years in some cases. This phase resolves on its own. The non-progressive phase is treated by surgical intervention.
- During management of TED, thyroid function evaluations are best done with the Thyroflex Test instead of the conventional Thyroid Blood Test that only measures the levels of thyroid hormones in the blood
INTRODUCTION: Clinical Presentation and Disease Overview
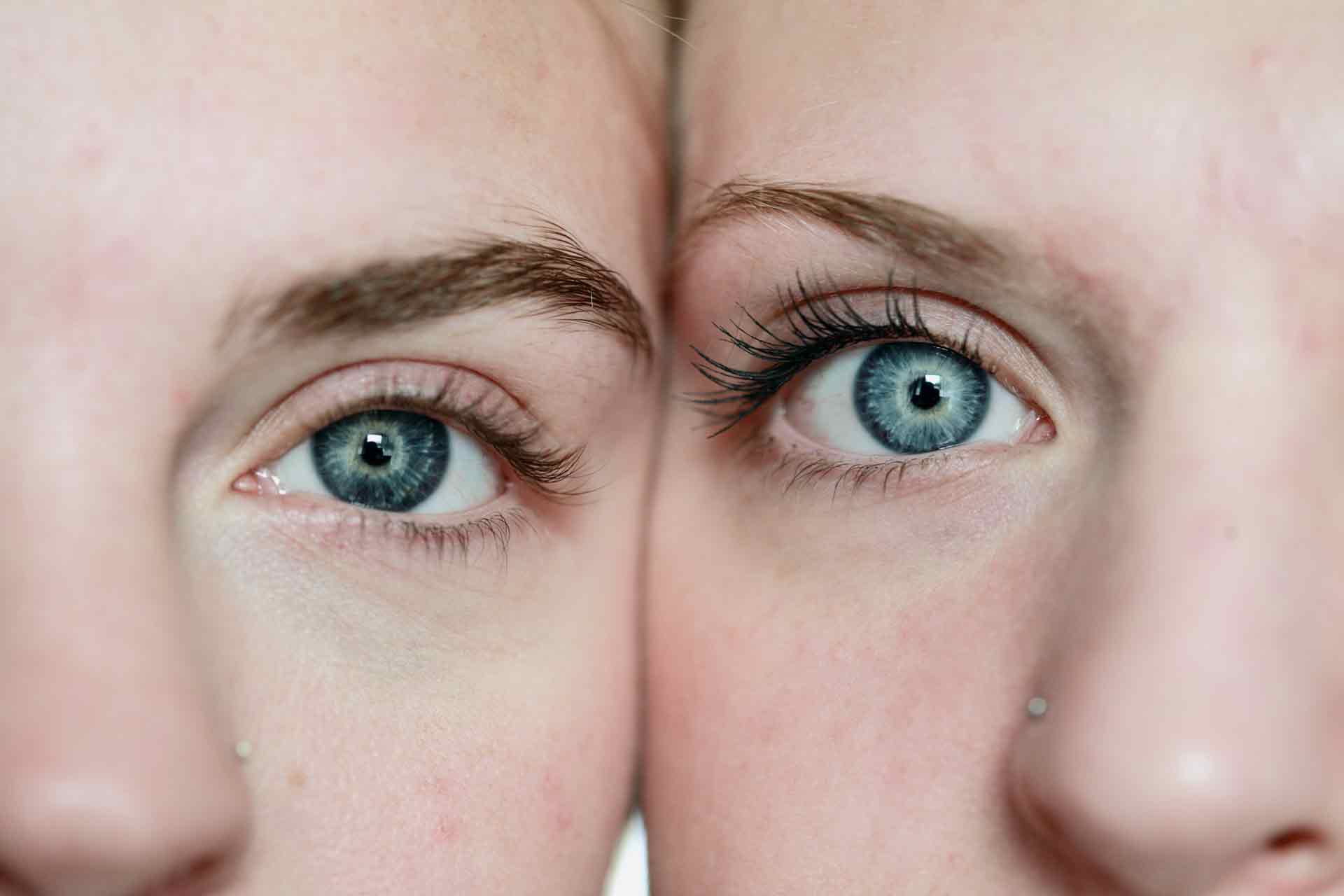
Normal thyroid functioning is an essential need in human biology as the Thyroid gland is directly linked with normal growth, cellular maturation and regulation of metabolism. The range of complications associated with thyroid dysfunctions can be debilitating, especially in cases of inadequate medical care. Thyroid Eye Disease (TED) describes a medical condition linked closely with autoimmune thyroid disease and characterized by periorbital edema (puffy eyes) , proptosis –abnormal protrusion of the eye, upper eyelid retraction, conjunctival injection, and chemosis –swelling of the conjunctiva. Also known as ‘Graves’ opthalmopathy, the presenting features of this disease are described by medical experts as a ‘Complex Orbital Inflammation’ with sight threatening and facial disfiguring effects.
Patients with an untreated or worsening case of Graves’ disease have a great tendency to develop TED –some medical reviews have described TED as the ocular manifestation of Graves’ disease. However, this disease has also been documented to be associated with Hashimoto’s thyroiditis, thyroid carcinoma, primary hypothyroidism and primary hyperthyroidism. With a predominant occurrence in females –associated with higher predisposition of hyperthyroidism in females, TED is estimated to have an incidence of 16 per 100,000 females and 2.9 cases per 100,000 males with no particular ethnic predisposition.
The disease course spans through two different phases. At the onset, the active disease phase is characterized by a recurrent unexplained bout of inflammatory reactions that can last for a few months or years in some cases. At the stage, there is a significant deposition of glycosaminoglycan in the extraocular muscles. Facial disfigurement, optic nerve depression, corneal diseases and associating signs develops gradually. The active phase is self-limiting, and develops in a non-progressive phase where the recommended therapy is based on surgical intervention.
The pathogenesis of Thyroid Eye Disease is not clearly defined, however, clinical findings have suggested retro-orbital inflammation caused mainly by increased orbital fibroblast activation as the most likely pathological explanation for TED. The inflammatory mediators directly induce swelling and redness of the periorbital tissues including the eyelids and conjunctiva. Consequently, there is an increase in the number of fat cells and fibroblasts. The increased secretion of glycosaminoglycan (connective tissue) leads to a cascade event of orbital volume expansion, congestion of orbital structures and abnormal protrusion of the eyeballs. Autoreactive T lymphocytes and B lymphocytes (immune response) invade and react with autoantigens (immune system) in the orbital soft tissues and extraocular muscles to trigger an inflammatory reaction –an autoimmune response in TED that is sustained by TSH receptor antibodies.
Symptom manifestation in patients with TED are non-uniform and depends on disease course and severity. The predominant symptoms expressed in the active phase of the disease include excruciating pain, reddening of the eyes, undue lacrimation (Tears) , photophobia (intolerance to light) , dry eyes, diplopia (double vision) and partial loss of vision. At the later phase, symptoms are more debilitating and can include chemosis, conjunctival injection, lid retraction, proptosis, eye movement restrictions and periorbital swelling.
Current Diagnosis Approach and Treatment Method
On presentation of the symptoms suggesting the onset of Thyroid eye disease, the clinicians investigate the level of normal functioning of the thyroid. For over decades, the levels of TSH, T4, free T4, and free T3 are considered a true indication of thyroid health. In the diagnosis of TED, the presence of thyroid auto-antibodies including anti-TSH receptor, anti-thyroid peroxidase (TPO) and anti-Tg antibodies are also determined. These findings were mostly done with the Thyroid Blood Test. However, the findings of Dr. David Derry have revealed that there exists no tangible connection between the signs and symptoms of thyroid disease and the levels of TSH or other biomarkers detected with the thyroid blood test.
As noted in the submissions of Dr. Richard Bayliss, about 75% of the thyroid hormones are found in the skin, muscles and brain, with a meagre 18% found in the blood. This invariably invalidates the long-term practice of clinicians to evaluate thyroid function with a blood test. Thy Thyroflex test has been considered the gold standard in evaluating thyroid health. This test measures the rate of conduction of impulses through the nerves and combines this with symptom presentation and the Resting Metabolic Rate to accurately diagnose the presence and severity of thyroid impairment, if any.
In some complicated cases where Thyroid function tests are inconsistent with symptom presentation, TED diagnosis a computer tomography (CT) scan can also be confirmed with orbital imaging –to check for inflammation and spared tendons suggestive of an active disease. Visual field analysis, orthoptic assessment and optometric assessment are also recommended.
Treatment Protocol for Thyroid Eye Disease
Currently, the management of TED is based on disease stage and severity. Researches have established the importance of anti-oxidants in the symptomatic management of mild active TED. Selenium supplements are the most widely recommended antioxidant therapy for TED. In 2011, a medical review published by the New England Journal of Medicine detailed the results of a randomized, double-blind, placebo-controlled trial in a bid to evaluate the effect of selenium in patients with Thyroid Eye Disease. An overall ophthalmic assessment carried 6 months after therapy initiation showed an improved quality of life and decreased progression of the disease. Other researches have suggested that selenium supplements at the right dose stops disease progression to the non-progressive stage.
The risk of vision loss is decreased by ensuring proper ocular lubrication with artificial tears, ointments and topical cyclosporine. Systemic corticosteroids are also indicated in the active phase of the disease as visual field defects and afferent papillary defects set in. Surgical intervention is considered the therapy option for TED at the non-progressive stage. Orbital decompression surgery is needed to manage optic neuropathy. Immunomodulatory therapy and Radiation therapy are also considered viable management options for TED especially in cases resistant to corticosteroid regimen.
REFERENCES
- www.ncbi.nlm.nih.gov/pmc/articles/PMC3711216/#!po=32.1429
- www.ncbi.nlm.nih.gov/pubmed/21591944
- www.ncbi.nlm.nih.gov/pmc/articles/PMC5384127/#!po=13.1356
- www.ncbi.nlm.nih.gov/pmc/articles/PMC3711216/#!po=27.6316
- www.thyroflex.com
- www.medscape.com/viewarticle/806399
- www.medscape.org/viewarticle/722615_2