Follicular Thyroid Cancer
OPENING SUMMARY
- Follicular Thyroid cancer constitutes about 15% of all diagnosed cases of Thyroid dysfunction, with the bulk of diagnosis recorded in regions of the world with low levels of iodine intake.
- A study published in 2011 by Oncologist has established a link between the development of ATC and the genetic make-up of patients diagnosed with the disease. Oncogene activation and a paired box PAX8-PPARy (8 Peroxisomes proliferator-activated receptor gamma) gene rearrangement occur in most cases of ATC
- This differentiated form thyroid cancer occur with variable level of severity and symptom presentation that depends on the disease variant –minimally invasive and invasive.
- Diagnosis is done with a Fine Needle Aspiration Biopsy with symptom assessment and thyroid function tests. The Thyroflex test has shown a 97% accuracy in providing a true assessment of thyroid function. This test objectively evaluates cellular function by measuring the speed of nerve impulse conduction through nerves and muscle cells.
INTRODUCTION: Clinical Presentation and Disease Overview
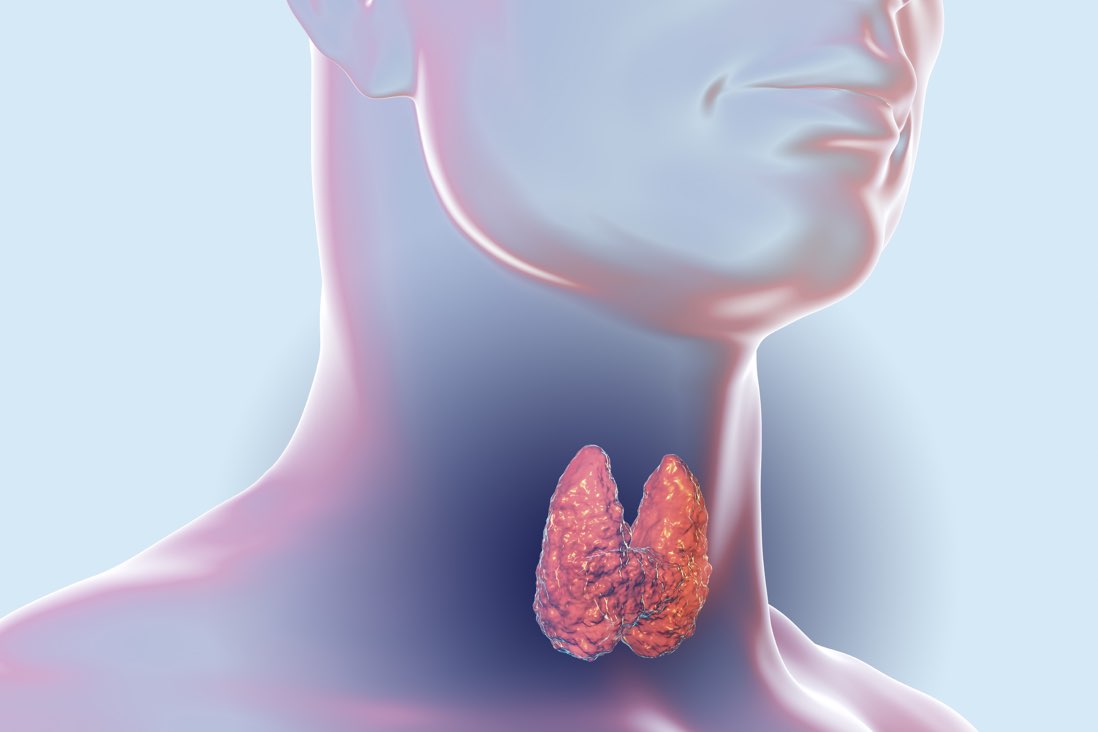
Thyroid cancers are generally studied and classified with focus on symptom spectrum and disease course severity. As published in the WHO’s Classification of Tumors of Endocrine Glands, follicular thyroid cancer is defined as ‘A malignant epithelial tumor showing follicular cell differentiation and lacking the diagnostic nuclear features of papillary thyroid carcinoma’ This widely accepted classified as a differentiated form of thyroid cancer is in a sharp contrast to anaplastic thyroid cancer which is considered ‘undifferentiated’.
With papillary thyroid cancer and anaplastic thyroid cancer, follicular thyroid cancer (FTC) requires a proper management plan when diagnosed. In all cases of thyroid cancer presentation, follicular thyroid cancer is the second most common, constituting about 15% of all diagnosis. About 40% of all cases are diagnosed in iodine-deficient regions of the world. In comparison with other forms, follicular thyroid cancer presents with an aggressive disease course and a more pronounced malignancy: differentiated cancerous cells are more likely to spread beyond the lymph nodes and invade distant organs through the blood stream.
With regards to morphologic presentation of the disease, follicular thyroid cancer is subdivided into to variants –minimally invasive and invasive. Occurring mostly in young patients, the minimally invasive variant is less malignant and presents as an encapsulated tumor without vascular invasion –tumor penetration into blood vessels within or outside the thyroid parenchyma, in this case. The invasive variant presents as a highly malignant tumor with evidences of vascular invasion beyond the tumor capsule into distant organs.
The pathogenesis of follicular thyroid cancer is not definite in description and involves a multi-factor hypothesis depending on disease severity and presentation. Iodine deficiency is considered a major risk factor in the development of FTC especially in patients older than 45 years. According to a study published in 2011 by Oncologist, Oncogene activation causing point mutations in the RAt Sarcoma (RAS) gene, and a paired box PAX8-PPARy (8 Peroxisomes proliferator-activated receptor gamma) gene rearrangement occur in about 40% of all confirmed diagnosis of follicular thyroid cancer. Through a complex cascade of biological responses, these mutations and rearrangements significantly reduces the effect of growth inhibitory controls and an eventual tumor development.
In most patients with follicular thyroid cancer, examination of the thyroid gland reveals a single palpable thyroid nodule with thyroiditis or nodular hyperplasia. Some cases, however, presents with no thyroid nodule. Thyroid functioning might be normal (Euthyroid state) in the minimally invasive variant. Continuous nodular development increases tumor size and predisposes patients to dyspnea, recurrent cough episodes, voice hoarseness, difficulty in swallowing and different episodes of choking spells that requires immediate intervention in critical cases. Some patients may also present with clinical symptoms suggesting hyperthyroidism with an accompanying complaint of neck pain.
Current Diagnosis Approach and Treatment Method
The generally acceptable golden standard for the diagnosis of thyroid malignancies including follicular thyroid cancer is a routine fine needle aspiration biopsy – expert examination and subsequent ultrasound examination of the thyroid gland. A positive diagnosis of FTC with fine needle aspiration biopsy reveals multiple follicular epithelial sheets overlapping in layers with microfollicle formation. Thyroid ultrasonography is particularly important in the diagnosis of follicular thyroid cancer as it can directly determine presence of nodules or calcifications. However, in cases where a more precise diagnosis is needed to guide therapy plan, this imaging study is inefficient in differentiating between the variants of the follicular thyroid malignancy.
Thyroid function tests are recommended for a more precise diagnosis when required. This tests include a complete workup of thyroid function in the presence of thyroid lumps. The levels of thyroid stimulating hormone, thyroxine and triiodothyronine are measured and compared with a reference range. This comparison can offer the clinician an idea of follicular tumor vascular invasiveness. Some clinicians have also suggested that levels of thyroglobulin (TG) antibodies be determined. In many diagnostic centers today, thyroid function tests are popularly balanced on the controversial Thyroid Blood Test. This test has however been judged inaccurate, and at best only indicative of an onset of thyroid dysfunction.
According to the 1971 findings of the famous Endocrinologist, Dr R.I.S Bayliss, TSH is a poor indicator of thyroid function. This submission is supported by the finding of Dr David Berry as documented in his book, ‘Breast Cancer and Iodine’. In his book, Dr David Berry concluded that an adequate test for Thyroid hormone levels should not be done by clinical assessment of blood tests as there is no confirmed relation between the signs and symptoms of low thyroid disease, TSH levels and blood tests. The Thyroflex test has shown a 97% accuracy in providing a true assessment of thyroid function. This test objectively evaluates cellular function by measuring the speed of nerve impulse conduction through nerves and muscle cells.
Treatment Protocol for Anaplastic Thyroid Cancer
A careful workup of symptoms presentation and disease severity –assessed based on vascular invasion –is needed to formulate an efficient management plan. Integrative therapy involving conservative surgical intervention has long been recommended by different medical experts. In cases where only a lobe of the thyroid has shown signs of nodular development, partial thyroidectomy removes the affected section. The incidence of tumor development in the opposite lobe of the thyroid tissue is increased by a diagnosis of nodule in the other tissue. This makes a case for Total Thyroidectomy –the removal of tumor cells from both lobes. Generally, Total Thyroidectomy is recommended in patients above 40 who presents with wide vascular invasion and/or bilateral nodular formation.
A follicular thyroid cancer management study published by the Clayman Thyroid Cancer Center has proposed that a Thyroidectomy procedure should be followed by radioiodine therapy and a thyroid suppression plan. Exogenous thyroid hormone is administered in these patients. Resultantly, the administered dose suppresses the levels of TSH and significantly reduces the possibility of cancer cell growth and restore normal thyroid functioning.
As a follow up plan, levels of the thyroid hormones are assessed at intervals to monitor thyroid functioning and therapy effectiveness. In many cases, a high thyroglobulin level after surgical intervention or TSH suppression is considered indicative of a recurrence. Far beyond Thyroid Blood Tests for hormone level assessments, the Thyroflex test is considered a more accurate follow up plan to assess thyroid functioning.
REFERENCES
- www.thyroidcancer.com/thyroid-cancer/follicular
- emedicine.medscape.com/article/278488-treatment#d8
- www.ncbi.nlm.nih.gov/pmc/articles/PMC3228182/#!po=10.3261
- www.ncbi.nlm/nih.gov/m/pubmed/31617165/#
- www.thyroflex.com